Predicting the spatiotemporal diversity
of seizure propagation and termination
in human focal epilepsy
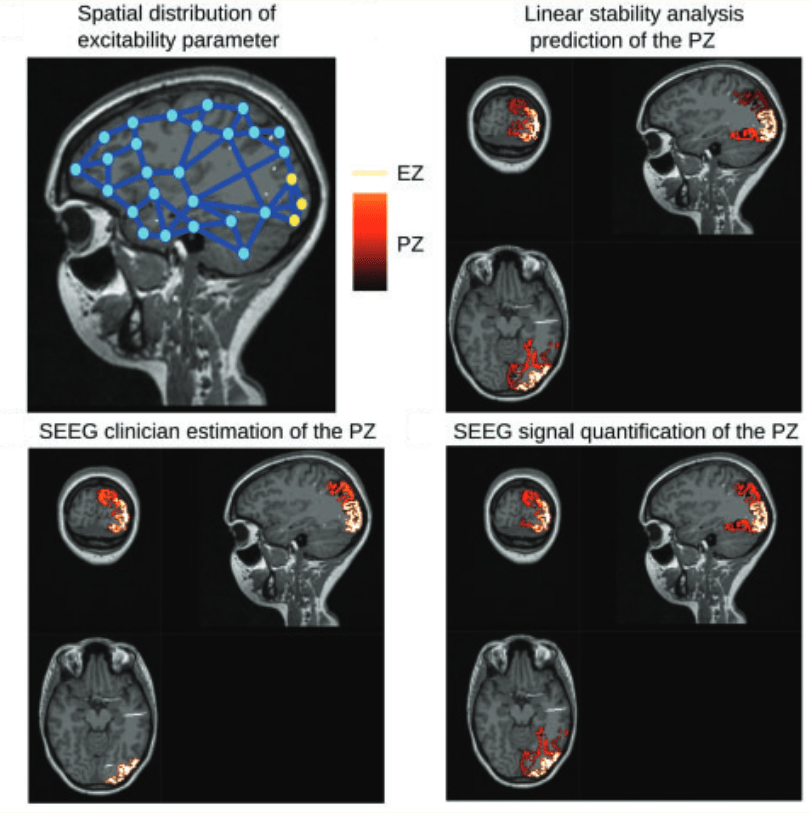
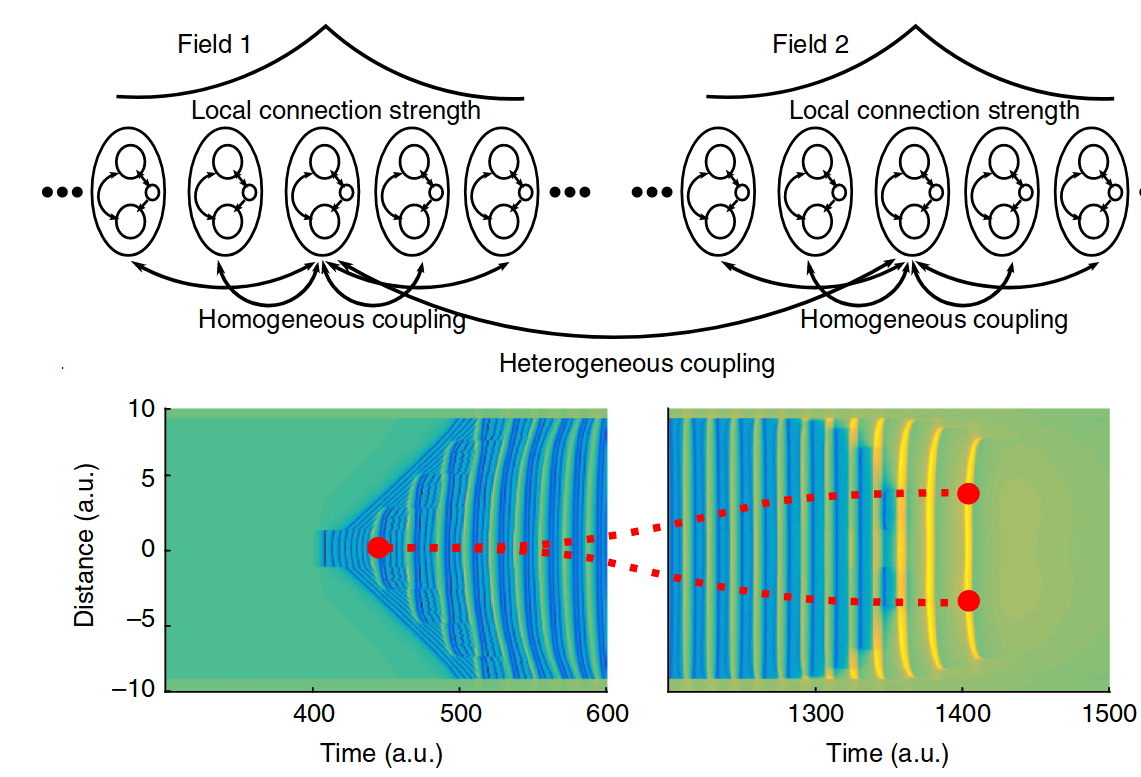
Recent studies have shown that seizures can spread and terminate across brain areas via a rich diversity of spatiotemporal patterns. In particular, while the location of the seizure onset area is usually invariant across seizures in an individual patient, the source of traveling (2–3 Hz) spike-and-wave discharges during seizures can either move with the slower propagating ictal wavefront or remain stationary at the seizure onset area. Furthermore, although many focal seizures terminate synchronously across brain areas, some evolve into distinct ictal clusters and terminate asynchronously. Here, we introduce a unifying perspective based on a new neural field model of epileptic seizure dynamics. Two main mechanisms, the co-existence of wave propagation in excitable media and coupled-oscillator dynamics, together with the interaction of multiple time scales, account for the reported diversity. We confirm our predictions in seizures and tractography data obtained from patients with pharmacologically resistant epilepsy. Our results contribute toward patient-specific seizure modeling.
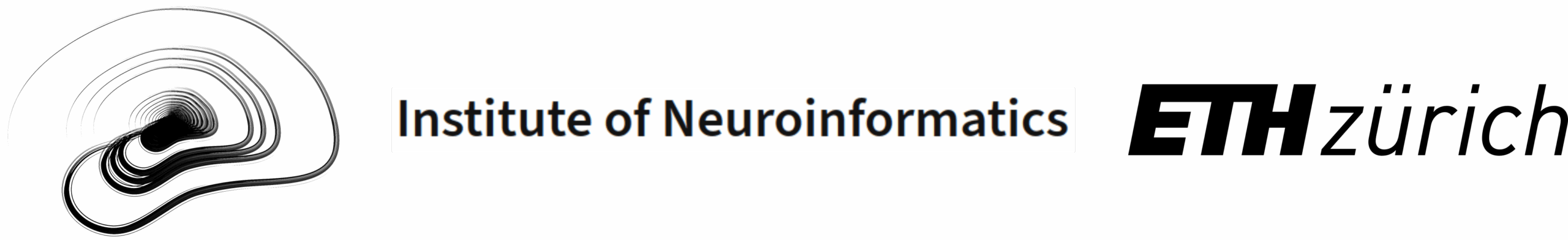
Individual brain structure and modelling
predict seizure propagation
Neural network oscillations are a fundamental mechanism for cognition, perception and consciousness. Consequently, perturbations of network activity play an important role in the pathophysiology of brain disorders. When structural information from non-invasive brain imaging is merged with mathematical modelling, then generative brain network models constitute personalized in silico platforms for the exploration of causal mechanisms of brain function and clinical hypothesis testing. We here demonstrate with the example of drugresistant epilepsy that patient-specific virtual brain models derived from diffusion magnetic resonance imaging have sufficient predictive power to improve diagnosis and surgery outcome. In partial epilepsy, seizures originate in a local network, the so-called epileptogenic zone, before recruiting other close or distant brain regions. We create personalized large-scale brain networks for 15 patients and simulate the individual seizure propagation patterns. Model validation is performed against the presurgical stereotactic electroencephalography data and the standard-of-care clinical evaluation. We demonstrate that the individual brain models account for the patient seizure propagation patterns, explain the variability in postsurgical success, but do not reliably augment with the use of patient-specific connectivity. Our results show that connectome-based brain network models have the capacity to explain changes in the organization of brain activity as observed in some brain disorders, thus opening up avenues towards discovery of novel clinical interventions.
https://doi.org/10.1093/brain/awx004
The Virtual Epileptic Patient:
Individualized whole-brain models
of epilepsy spread
Individual variability has clear effects upon the outcome of therapies and treatment approaches. The customization of healthcare options to the individual patient should accordingly improve treatment results. We propose a novel approach to brain interventions based on personalized brain network models derived from non-invasive structural data of individual patients. Along the example of a patient with bitemporal epilepsy, we show step by step how to develop a Virtual Epileptic Patient (VEP) brain model and integrate patient-specific information such as brain connectivity, epileptogenic zone and MRI lesions. Using high-performance computing, we systematically carry out parameter space explorations, fit and validate the brain model against the patient’s empirical stereotactic EEG (SEEG) data and demonstrate how to develop novel personalized strategies towards therapy and intervention.
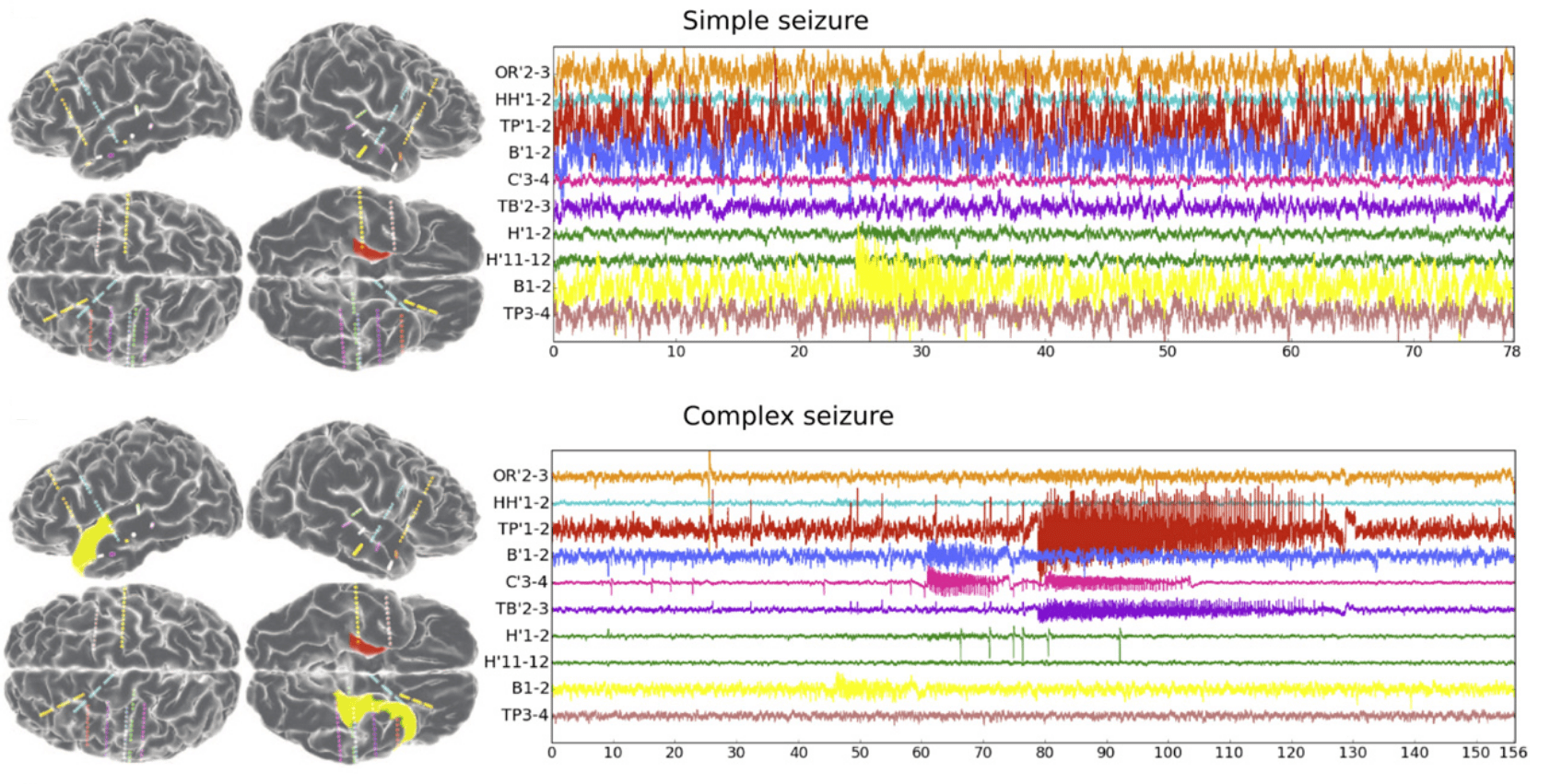
Permittivity coupling across brain regions
determines seizure recruitment
in partial epilepsy
Brain regions generating seizures in patients with refractory partial epilepsy are referred to as the epileptogenic zone (EZ). During a seizure, paroxysmal activity is not restricted to the EZ, but may recruit other brain regions and propagate activity through large brain networks, which comprise brain regions that are not necessarily epileptogenic. The identification of the EZ is crucial for candidates for neurosurgery and requires unambiguous criteria that evaluate the degree of epileptogenicity of brain regions. To obtain such criteria and investigate the mechanisms of seizure recruitment and propagation, we develop a mathematical framework of coupled neural populations, which can interact via signaling through a slow permittivity variable. The permittivity variable captures effects evolving on slow timescales, including extracellular ionic concentrations and energy metabolism, with time delays of up to seconds as observed clinically. Our analyses provide a set of indices quantifying the degree of epileptogenicity and predict conditions, under which seizures propagate to nonepileptogenic brain regions, explaining the responses to intracerebral electric stimulation in epileptogenic and nonepileptogenic areas. In conjunction, our results provide guidance in the presurgical evaluation of epileptogenicity based on electrographic signatures in intracerebral electroencephalograms.
https://doi.org/10.1523/JNEUROSCI.1570-14.2014